What is Stage II Melanoma?
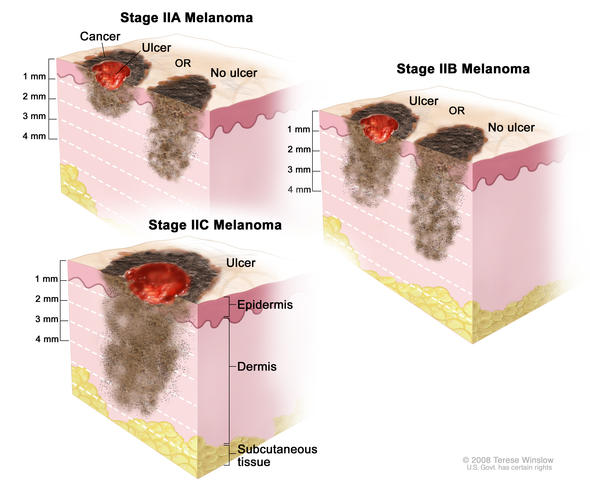
In Stage II melanoma, the cancer cells are in both the first layer of skin—the epidermis—and the second layer of skin—the dermis. The melanoma is higher risk than Stage I, either due to depth of tumor or presence of ulceration, but there is no evidence the cancer has spread to lymph nodes or distant sites (metastasis). Stage II melanoma is local melanoma, meaning it has not spread beyond the primary tumor. There are three subgroups of Stage II melanoma: IIA, IIB, and IIC. Stage II melanoma is invasive melanoma, as are Stage I, III, and IV; Stage 0 is not considered invasive melanoma.
Subgroups are IIA, IIB, IIC
- Stage II melanoma is defined by tumor thickness (Breslow Depth) and ulceration
- There is no spread to nearby lymph nodes or distant sites
- Risk: intermediate to high for regional or distant spread
Characteristics of Stage II Melanoma
Stage II melanomas are defined by two primary characteristics: tumor thickness and ulceration.
Tumor thickness (Breslow Depth): how deeply the tumor has penetrated the skin. Thickness is measured in millimeters (mm). These comparisons will give you an idea of size:
- 1 mm = .04 inch, or less than 1/16 inch—about equal to the edge of a penny
- 2 mm = between 1/16 and 1/8 inch—about equal to the edge of a nickel
- 4 mm = between 1/8 and 1/4 inch—about equal to the edges of two nickels
Ulceration: when the epidermis (or top layer of skin) that covers a portion of the primary melanoma is not intact. Ulceration can only be seen under a microscope, not by the naked eye.
Subgroups of Stage II Melanoma
There are three subgroups of Stage II melanoma:
Stage IIA
The tumor is 1.01 – 2.0 mm thick, with ulceration, OR tumor is 2.01 – 4.0 mm thick, without ulceration.
There is no evidence of spread to nearby lymph nodes.
There is no evidence of metastasis to distant sites.
Stage IIB
The tumor is 2.01 – 4.0 mm thick, with ulceration, OR tumor is greater than 4.0 mm thick, without ulceration.
There is no evidence of spread to nearby lymph nodes.
There is no evidence of metastasis to distant sites.
Stage IIC
The tumor is greater than 4.0 mm thick, with ulceration.
There is no evidence of spread to nearby lymph nodes.
There is no evidence of metastasis to distant sites.
Risk: With treatment, Stage II melanoma is considered intermediate to high risk for local recurrence or for regional and distant metastases.
Treatment Options for Stage II Melanoma
Treatment of Stage II melanoma can include surgery, sentinel lymph node biopsy, immunotherapy, and clinical trials.
Surgery
The standard treatment for Stage II melanoma is surgery, called wide local excision. The purpose of the surgery is to remove any cancer remaining after the biopsy.
In a wide local excision, the surgeon removes any remaining tumor from the biopsy site, the surgical margin (a surrounding area of normal-appearing skin), and the underlying subcutaneous tissue, to make certain the whole tumor has been removed.
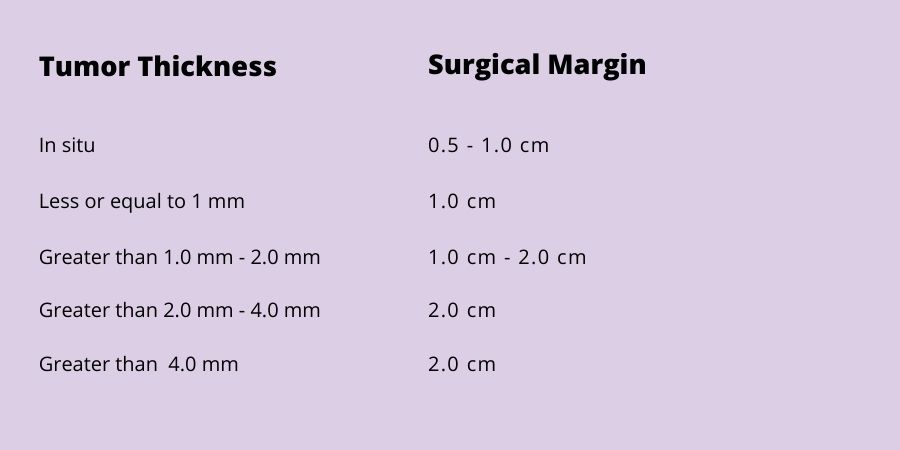
The width of the margin taken depends upon the thickness of the primary tumor. The surgical margin guidelines adopted and recommended by the National Comprehensive Cancer Network (NCCN) for wide local excision of primary melanomas range from 0.5 cm to 2 cm:
Options For Stage II Melanoma: Making the Decision that’s Right For You
On behalf of AIM, Dr. Geoffrey Lim, a dermatologic surgeon in private practice at SkinMed Institute in Lone Tree, Colorado, interviewed Dr. Jason Luke, Associate Professor of Medicine at the University of Pittsburgh Medical Center, a leading medical oncologist and one of the authors of a key adjuvant therapy study. They discussed the most common questions about Stage II melanoma, which Stage II patients are eligible for adjuvant therapy, and the pros and cons of adjuvant therapy vs active surveillance. This resource should help you, your loved one, and your oncology care team make an informed decision about steps to take after surgery.
Sentinel Lymph Node Biopsy (SLNB)
SLNB is performed to determine whether any cancer cells have spread to the sentinel node, the first lymph node to receive drainage from the primary tumor, and the site where melanomas commonly spread to first. Sentinel lymph node biopsy is recommended for all Stage II tumors regardless of size.
SLNB is most accurate when the lymph channels around the primary melanoma have not been disturbed by a prior wide local excision. Therefore, in most cases, if you are having an SLNB, your SLNB and wide local excision are performed in succession, with the SLNB performed first.
If your SLNB is positive, you will be diagnosed with Stage III melanoma. Read here for more on Stage III melanoma. If your SLNB is negative, your diagnosis will remain Stage II. It is recommended that Stage IIB and IIC patients see a medical oncologist, as there is an approved treatment for Stage IIB and IIC, as well as ongoing clinical trials. Your doctor may recommend treatment.
If you are Stage IIA, your doctor will recommend observation—monitoring you closely for signs of recurrence—as your next step.
Immunotherapy
Keytruda (pembrolizumab), an immunotherapy, is approved for use in Stage IIB and IIC patients with melanoma who are 12 years and older, following complete resection of the melanoma. The approval is based upon the results of a Phase 3 clinical trial involving 976 newly diagnosed patients in which Keytruda showed a statistically significant improvement in recurrence-free survival (RFS), reducing the risk of disease recurrence or death by 35% compared to placebo alone.
Opdivo (nivolumab), an immunotherapy, is approved for the adjuvant treatment of completely resected Stage IIB and Stage IIC melanoma in patients 12 years and older. The approval is based upon the results of a Phase 3 trial involving 790 newly diagnosed patients. In the trial, Opdivo reduced the risk of recurrence, new primary melanoma, or death in patients with completely resected Stage IIB or Stage IIC melanoma by 58% compared to placebo alone.
Clinical Trials
Clinical trials are research studies to evaluate new therapies and improve cancer care. These studies are responsible for most of the advances in cancer prevention, diagnosis, and treatment. If you have melanoma, you may be eligible to participate in a clinical trial. Several treatments for Stage IV melanoma are currently being tested in clinical trials for Stage II:
- Immunotherapy and immunotherapy combinations designed to boost the immune system to fight the return of melanoma.
- Targeted therapies and targeted therapy combinations that work by blocking the function of the mutated BRAF protein
- Vaccines that may improve the specific immune response to melanoma
What to Ask Your Doctor about Stage II Melanoma
When your doctor tells you that you have Stage II melanoma, it can be overwhelming. But it is important to use the time with your doctor to learn as much about your cancer as you can. S/he will provide you important information about your diagnosis.
It is often helpful to bring a friend or family member with you to your doctor’s appointment. This person can lend moral support, ask questions, and take notes.
The following questions are those you may want to ask your doctor. Remember, it is ALWAYS okay to ask your doctor to repeat or clarify something s/he has said so that you can better understand it. You may find it helpful to print out these questions and bring them with you to your next appointment.