How Do You Take Care of a Melanoma Patient’s Psychological Needs?
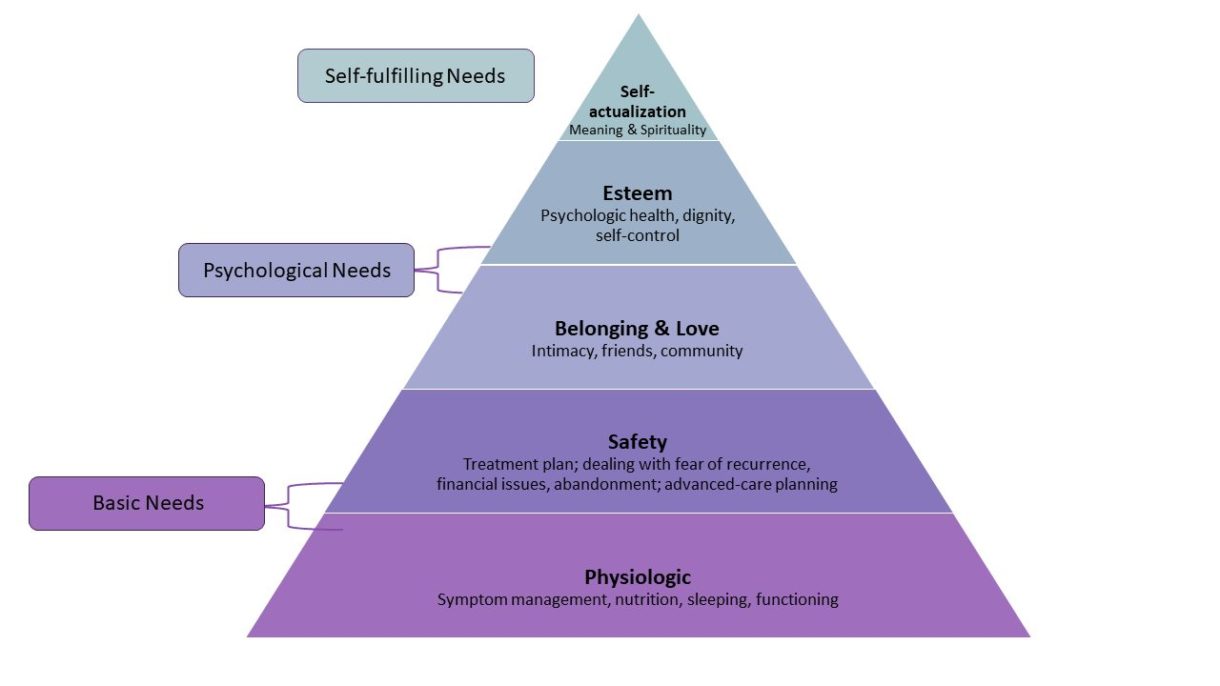 Cancer patients will have Psychological Needs—those relating to both the patient’s external relationships and internal state of being—and you, the caregiver, can help tend to those needs. We’ll first discuss the need for belonging and love and then the need for esteem.
Cancer patients will have Psychological Needs—those relating to both the patient’s external relationships and internal state of being—and you, the caregiver, can help tend to those needs. We’ll first discuss the need for belonging and love and then the need for esteem.
Psychological Needs: Helping Your Loved One Feel Belonging & Love
Those with melanoma may be concerned about their role in their family, their intimate relationship, and where they fit in. They may also be worried about how their family is going to function while they are unwell or if they die. As a caregiver, you will likely help your loved one deal with these concerns, and you may have similar concerns of your own.
Family Dynamics
Some strategies have been found to be helpful for families dealing with cancer:
- Getting the family together in a family conference mediated by a health professional
- Sharing care support roles among family members. Sharing support roles help ensure the person with cancer receives the necessary emotional and logistical support without overlooking a particular family member, which, in turn, can reassure the person with cancer. Consider using the Lotsa App
- Sharing information among family members openly and in a timely manner. There are communication tools to help with this process, such as CaringBridge
Each family has its own family and relationship dynamics as well as communication strategies and roles. It’s important to understand that these dynamics, strategies, and roles may shift with the melanoma diagnosis. As you develop things such as new communication strategies, keep in mind that the patient, yourself, and other family members may have personal preferences or cultural expectations about sharing information and talking about the disease. Or the person with melanoma may not want to cause more stress for the remainder of the family by talking about the disease. However, no matter what the communication strategy is, your loved one should never be left out of communications with the healthcare team. If you, as a caregiver, have something to share with the oncology team, it’s best to bring it up with the patient there. In fact, the patient should guide the level of your involvement. If your loved one does not feel like s/he has a say, it can lead to a lot of unnecessary frustration and a break down in the relationship with the oncology team.
How does a caregiver deal with a difficult patient? Melanoma can be a roller coaster ride, and emotions run high. As a caregiver, you may reach a point where you want to quit if your loved one is inadvertently driving you crazy.
Some general principles that help when dealing with a difficult person include[i]
- Accept that it’s not you
- Don’t take it personally
- Redirect the person
- Acknowledge the person’s concern
- Get help from the healthcare provider
- Get support for yourself in your caregiving role
- Find outlets for the person to connect
- Stand up for yourself (you love this person, but you will not tolerate bad behavior)
And I did.
I wanted to get all the information I could on it.”
Celeste M., caregiver
Talk To Our Melanoma Medical Expert
Sense of Belonging
It’s important for patients with melanoma to feel like they are still part of the family. Your loved one should be reassured that s/he is still a contributor and should be involved with normal family activities as much as possible. Roles may need to shift at different stages of the melanoma journey; however, it is important to make sure the person with melanoma still feels valued. Some members of the family will feel the need to be protective of the patient and may have guilt about asking anything from the patient. But being able to contribute to the family, even in a reduced capacity, can be helpful for a melanoma patient’s sense of self-esteem. Doing loving things for their family members can give melanoma patients a sense of control and make them feel more like themselves. It’s important to let them fulfill those roles.
Intimacy Needs
Melanoma can affect intimate relationships for a number of reasons. Surgeries can leave scars that can be disfiguring. If radiation therapy is involved, it can also leave unattractive sores. The melanoma treatments themselves can have sexual side effects. In the case of immunotherapy, the fatigue and potential hormonal impact can pose a challenge to intimacy. Other irAEs such as skin toxicities or neurologic effects can also make intimacy challenging. In addition, the emotional aspects of the melanoma journey can affect both partners in a relationship. If you are a caregiver who is also the intimate partner of the patient, it is worthwhile addressing these concerns directly and with open communication. For more information about addressing the effect of cancer on intimate relationships, see ASCO’s pages on relationships and dating.
Another important intimacy consideration is the safety aspects of pregnancy and family planning during melanoma treatment. For patients receiving checkpoint inhibitors, there are specific requirements for avoiding pregnancy during treatment and for a period of time thereafter. These timeframes may differ depending on the specific drug(s) taken, but generally speaking, it’s best to wait six months before considering pregnancy after the last dose of checkpoint inhibitor therapy. Little is known about the impact of checkpoint inhibitors on fertility. The impact is likely to be complex because of the potential of long-term effects on the immune system from these drugs in both men and women. Side effects could occur (including hormonal changes such as pituitary or thyroid problems) that may require additional hormonal supplementation, thus affecting fertility. If you are the caregiver who is also the intimate partner of the patient, these considerations are important for both of you as you navigate melanoma and family planning.
It’s important for the person with melanoma to have a frank conversation with the oncology team about family planning issues prior to starting treatment. The patient might also want to consider seeing a fertility specialist who is familiar with these issues in cancer patients to discuss egg or sperm freezing. As the caregiver, you can help the patient broach these topics as part of the planning process.
Social Needs
Sometimes the social needs of the patient extend beyond the partner, family, and friend support systems. Melanoma patients may benefit greatly by talking with other melanoma patients and should be informed about options for support groups or peer-to-peer connections. While not everyone feels comfortable with these support models, patients should know about the option. It’s always a good idea to suggest to your loved one that s/he at least consider trying a session or two to see if the s/he finds benefit. These support groups can fulfill several roles for people with melanoma:
- Educating people and families about the disease
- Sharing the illness experience
- Providing strength and hope
- Raising public awareness about the disease
- Fundraising for research into the disease
The support groups may also provide a means for people with melanoma to give back when they are further along in their journey. This ability to give back can be helpful in the healing process and in finding meaning with the cancer experience. AIM has its own peer-to-peer support program called Peer Connect. Your oncologist’s office may have other options, too.
and it was nice to see my mom…being my mom.”
Lisa R, long-distance caregiver
Peer Support For Caregivers
Psychological Needs: Helping Your Loved One With Esteem
As mentioned, the diagnosis of melanoma and the melanoma journey can have a profound impact on the emotional status of the patient. And emotional status can affect how your loved one fares overall. In fact, when emotional issues are not addressed, they can reduce the patient’s quality of life, impair social relationships, increase the rehabilitation time, and affect adherence to treatment. These problems are common—about 50% of patients with cancer experience psychiatric problems, including severe emotional distress.[i] Unfortunately, many psychiatric issues in cancer patients go unrecognized or untreated. While there is increased emphasis on psycho-oncology as a mandatory component of comprehensive cancer care, as the caregiver you can assist the healthcare team in identifying signs of psychological distress and making sure the issues are addressed. Be as proactive as possible in communicating concerning issues to the oncology team. They will have options to help directly, or they may bring in experts to help.
Some signs of more serious distress in the patient are outlined by the American Cancer Society and include:
- Feeling overwhelmed or panicky
- Being overcome with dread
- Feeling sad to the point where the person with cancer thinks s/he no longer can go on with treatment
- Acting unusually irritable or angry
- Being unable to cope with pain, tiredness, and nausea
- Fuzzy thinking, poor concentration, memory issues
- Difficulty making decisions, even about small things
- Feeling a sense of hopeless
- Thinking about cancer and/or death constantly
- Experiencing trouble sleeping or getting less than 4 or 5 hours of sleep a night
- Having trouble eating for a few weeks
- Family conflicts and issues that seem impossible to resolve
- Questioning faith and beliefs that once gave you comfort
- Feeling worthless, useless, and like a burden to others
If your loved one appears to be experiencing any of the above, make sure you share this information with his or her oncology team and seek professional help.
It’s important to know that about 50% of patients with cancer experience psychiatric problems. These can include severe emotional distress. Many of these conditions go unrecognized or untreated. You, as the caregiver, can help to make sure your loved one’s mental health is also addressed.[ii]
Beyond seeking professional help, patients with melanoma can benefit from lifestyle changes that can reduce stress. In fact, usually, a combination of approaches is most beneficial. But in general, the approaches are similar to those strategies we can all use for stress-relief:
- Practice a breathing method
- Try meditation or yoga
- Make sure to get enough sleep
- Start an exercise routine
- Explore hobbies
- Eat well during treatment
- Seek light and humorous experiences
- Be social
By remaining actively engaged in life and exerting control over the things they can control, your loved one can hopefully achieve greater peace of mind and can enhance self-esteem. As the caregiver, you can help encourage lifestyle changes that reduce stress and enhance self-esteem.

