What is Translational Medicine?

By Maria Libera Ascierto, MS, PhD
Associate Professor Translational Cancer Immunology
Director “The Rosalie and Harold R Brown Cancer Immunotherapy” Program
Providence Saint John’s Cancer Institute
One issue in medicine is the lack of connection that can sometimes exist between the clinic—where patients are seen and treated—and the laboratory—where research is conducted. This lack of connection is often a translation problem: Promising laboratory discoveries need to be translated into clinical applications, and clinical questions need to be translated into laboratory research projects.
To address this gap, the term translational medicine was introduced in the 1990s thus gaining wide usage in the early 2000s. Originally, translational medical research emerged from a class of medical research called “bench-to-bedside” that aimed to transfer scientific knowledge more directly from the laboratory (bench) to patients (bedside) and vice versa.
In 2003, the Institute of Medicine’s Clinical Research Roundtable described the current terminology and model of translational research as a two-phase process of research, progressing from:
- basic science to clinical science; and
- clinical science to public health impact.
Currently, there is not a clear definition of translational medicine because this growing discipline means different things to different people.
However, I like to define translational medicine (also referred to as translational science) as biomedical research that aims to eliminate the barriers between laboratory and clinical practice and expedite the discovery in the laboratory of new diagnostic tools or treatments by using a multidisciplinary approach focused on the integration of basic research, clinical research, and patient-oriented research.
In other words, translational medicine converts promising laboratory discoveries into clinical applications and attempts to answer clinical questions with the use of laboratory research to facilitate prediction, prevention, diagnosis, and treatment of diseases. By doing so, translational medicine aims to transform the basic investigational achievements of medical biology into practical theory, technology, and methods that will bridge laboratory and clinical practice.
This means that translational medicine needs to follow a bi-directional workflow that encompasses:
- bench-to-bedside factors, which aim to increase the efficiency by which new therapeutic strategies developed through research are tested clinically on patients; and
- bedside-to-bench factors, which provide novel sources (patients’ specimens, patients’ feedback) which will be used by scientists to promote new treatments and discover new tools to help patients’ lives.
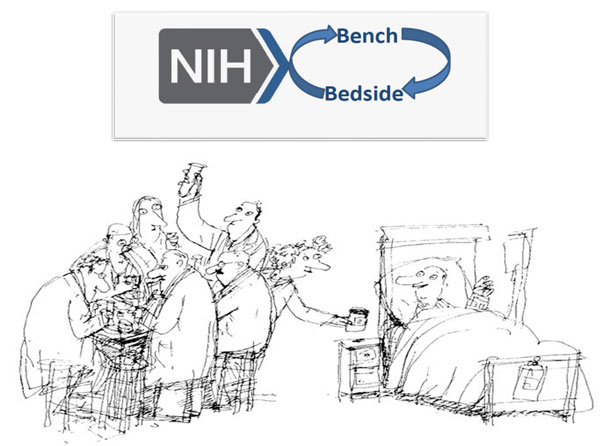
Source: National Institutes of Health (NIH) – bench to bedside program
Why is the patient’s contribution so important for translational medicine?
Translational medicine involves a more patient-centric approach to medicine than the traditional process. The role of the patient in this research is considered critical: Patients provide the biospecimens from which biomarkers at the molecular and immune level can be identified and are then used to develop diagnostics and drugs targeted at sub-groups of disease. Patients become the real heroes of translational medicine and the true protagonists of all the advances in novel therapeutic interventions.
It is important for the scientific community to remember to inform patients and their families of their critical involvement in translational medicine research and to also share with them all the successes achieved through their contributions.
What have we achieved with translational medicine in melanoma?
Recent progress in melanoma drug development highlights the critical impact that translational medicine plays in advancing the care of melanoma patients.
Prior to 2011, the treatment of melanoma was limited to the usage of dacarbazine, interleukin (IL)-2, and interferon (IFN)α-2b for all patients with melanoma thus resulting in a relatively poor response.
A renaissance occurred when, with the usage of translational medicine approaches, it was discovered that many patients with melanoma harbor molecular alterations in the mitogen-activated protein kinase (MAPK) pathway. As result, any patients with melanoma harboring this mutation could be treated with compounds able to target the mutated pathway. Three directed consequences followed this discovery: 1) pharmaceutical companies vigorously pursued the development of treatment options able to inhibit the MAPK pathway; 2) in a very short period, the FDA approved the usage of three successful MAPK pathway inhibitors for the treatment of patients with advanced melanoma harboring mutations in MAPK pathway; and 3) thanks to translational medicine, the era of precision medicine, which fosters the usage of a specific drug for specific subsets of patients, just began!
To follow, additional advances in translational medicine led to the discovery that many patients with melanoma (or in general with cancer) are characterized by a dormient immune status, generated by overexpression of immune checkpoints such as PD(L)1 and CTLA4, which ultimately leads to a reduced immune action versus the cancer cells. The development of treatment options able to block those immune checkpoints, such as ipilimumab (Yervoy; a CTLA4 inhibitor), pembrolizumab (Keytruda; an anti-PDL1 inhibitor) and nivolumab (Opdivo; an anti-PD1 inhibitor) clearly generated a number of scientific breakthroughs (Topalian S et al, NEJM 2012; Brahmer J et al, NEJM 2012) thus completely changing the standard of care of patients with melanoma and other tumor types.
What is the current focus of translational melanoma research?
Currently, the focus of translational medicine research has taken a bidirectional route, focusing on:
- Exploring biomarkers able to better predict the efficacy of treatments already approved by the FDA to foster a more precise therapeutic intervention (Ascierto ML et al, Clinical Cancer Res 2017; Hugo W et al. Cell 2016).
- Exploring novel targets or pathways to generate novel treatments options that can be used either alone or in combinations to increase the overall response of patients with melanoma. To support this last aspect, multiple Phase 0 trials deeply focused on translational medicine questions to validate the Mechanisms of Actions (MoA) of selected novel therapeutic interventions are fostered by pharmaceutical companies.
Translational medicine has succeeded in connecting the bench (laboratory) and the bedside (clinic) and translating their needs to each other. In the next decade, even more successes in melanoma treatment are expected to be achieved thanks to translational medicine. But this will only be possible if a dedicated and continuous collaboration between patients, scientists and clinicians will continue to be in place.
Recent Posts

The Cost of Sunscreen May Be Costing Lives

A Conversation with Dr. Rena Szabo, PsyD on Empowering Patients

Empowering Women in Melanoma: A Look Inside the Women in Melanoma Initiative

Melanoma News and Highlights You Don’t Want to Miss


