What is Stage I Melanoma?
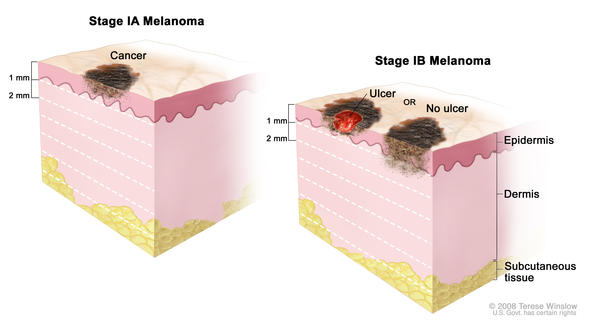
In Stage I melanoma, the cancer cells are in both the first and second layers of the skin—the epidermis and the dermis. A melanoma tumor is considered Stage I if it is up to 2 mm thick, and it may or may not have ulceration. There is no evidence the cancer has spread to lymph nodes or distant sites (metastasis). Stage I melanoma is local melanoma, meaning it has not spread beyond the primary tumor. Stage I melanoma is invasive melanoma, as are Stage II, III, and IV; Stage 0 is not considered invasive melanoma. There are two subgroups of Stage I melanoma: IA and IB.
Stage I: Melanoma “localized tumor”
- Subgroups are IA, IB
- Stage I melanoma is defined by tumor thickness and ulceration
- There is no spread to nearby lymph nodes or distant sites
- Risk: Low
Characteristics of Stage I Melanoma
Stage I melanomas are defined by two primary characteristics: tumor thickness and ulceration.
Tumor thickness (also called Breslow Depth): how deeply the tumor has penetrated the skin. Thickness is measured in millimeters (mm). These comparisons will give you an idea of size:
- 1 mm = .04 inch, or less than 1/16 inch—about equal to the edge of a penny
- 2 mm = between 1/16 and 1/8 inch—about equal to the edge of a nickel
Ulceration: when the epidermis (or top layer of skin) that covers a portion of the primary melanoma is not intact. Ulceration can only be seen under a microscope, not by the naked eye.
Subgroups of Stage I Melanoma
There are two subgroups of Stage I melanoma: Stage IA and Stage IB.
Stage IA and Stage IB melanoma has no evidence of spread to nearby lymph nodes, and no evidence of metastasis to distant sites.
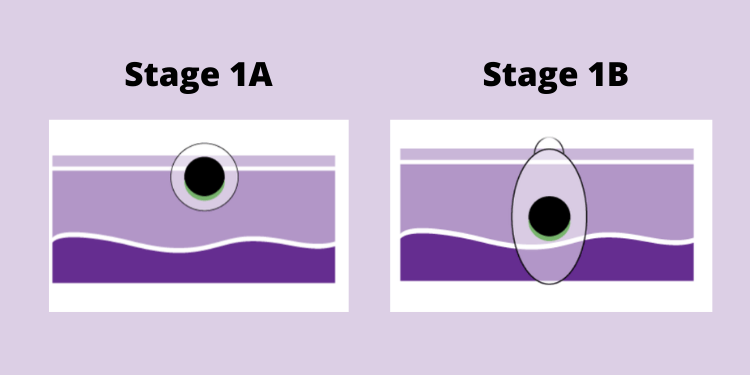
Stage IA and Stage IB are differentiated by depth of tumor and ulceration:
- Tumors that are less than 0.8 mm without ulceration are Stage IA.
- Tumors that are greater than 1.0 mm and up to 2.0 mm without ulceration are Stage IB.
- Tumors that are less than 0.8 mm with ulceration and tumors that are between 0.8 mm and 1.0 mm with or without ulceration are Stage IB; however,
- if you have a tumor in this category and undergo sentinel lymph node biopsy (SLNB; see more about SLNB below), and no evidence of lymph node metastasis is found, your new stage subgrouping is Stage IA. Why the difference? The former is the clinical stage, and the latter is the pathological stage. Stage can be defined at several different points in your cancer care, and new information can sometimes give you a new stage grouping. Clinical staging is the assessment of your melanoma after the original tumor biopsy, and pathological staging is the assessment after SLNB and wide local excision (WLE; see more about WLE below). In the case of these Stage I melanomas, the SLNB has ruled out evidence of spread to the lymph nodes, which means there’s a good indication that your melanoma is less risky, which is why the tumor is now assessed at Stage IA vs. IB. If you do not undergo SLNB, you do not have a pathological stage group, and your clinical stage group remains Stage IB.
Risk: Patients with Stage I melanoma are considered low risk for local recurrence or for regional and distant metastases.
Treatments for Stage I Melanoma
The standard treatment for Stage I melanoma is surgery, called wide local excision. The purpose of the surgery is to remove any cancer remaining after the biopsy. Your doctor may also perform a sentinel lymph node biopsy based on the risk of the tumor spreading.
Wide Local Excision
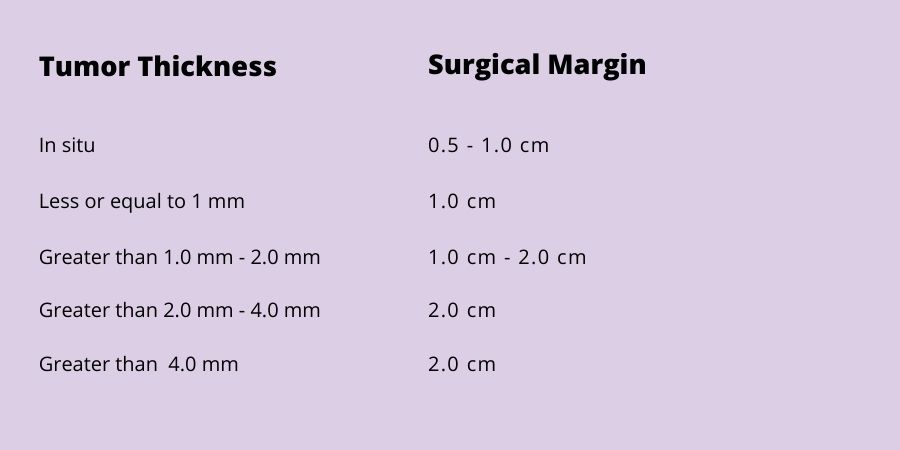
In a wide local excision, the surgeon removes any remaining tumor from the biopsy site, the surgical margin (a surrounding area of normal-appearing skin), and the underlying subcutaneous tissue, to make certain the whole tumor has been removed. This procedure may be done in a doctor’s office under local anesthetic.
The width of the margin taken depends upon the thickness of the primary tumor. The surgical margin guidelines adopted and recommended by the National Comprehensive Cancer Network (NCCN) for wide local excision of the primary melanoma range from 0.5 cm to 2 cm:
Sentinel Lymph Node Biopsy (SLNB)
The purpose of SLNB is to determine whether any cancer cells have spread to the sentinel node—the first lymph node to receive drainage from the primary tumor, and the site where melanoma commonly spreads to first.
Sentinel lymph node biopsy is most accurate when the lymph channels around the primary melanoma have not been disturbed by a prior wide local excision. Therefore, in most cases, if you are having an SLNB, your SLNB and wide local excision are performed in succession, with the SLNB performed first.
SLNB is recommended for patients with
- tumors greater than 1.0 mm thick
- tumors between 0.8 and 1.0 mm thick with additional adverse prognostic markers
- ulcerated tumors of any thickness
- positive biopsy margins
- lymphovascular invasion (cancer cells in the lymphatic channels or blood vessels)
Further treatment will depend on whether the lymph node biopsy is positive.
What to Ask Your Doctor about Stage I Melanoma
When your doctor tells you that you have Stage I melanoma, it can be overwhelming. But it is important to use the time with your doctor to learn as much about your cancer as you can. S/he will provide you important information about your diagnosis.
The following questions are those you may want to ask your doctor. Remember, it is ALWAYS okay to ask your doctor to repeat or clarify something s/he said so that you can better understand it. You may find it helpful to print out these questions and bring them with you to your next appointment.
