Melanoma ocular

¿Qué es el melanoma ocular?
Ocular melanoma Es una forma rara de melanoma que se presenta en el ojo. Aunque se desarrolla a partir de melanocitos, el mismo ARNm codificando (SCD por sus siglas en inglés), que causa melanoma en el piel, debe considerarse un asunto separado células cancerosas por melanoma de la piel.
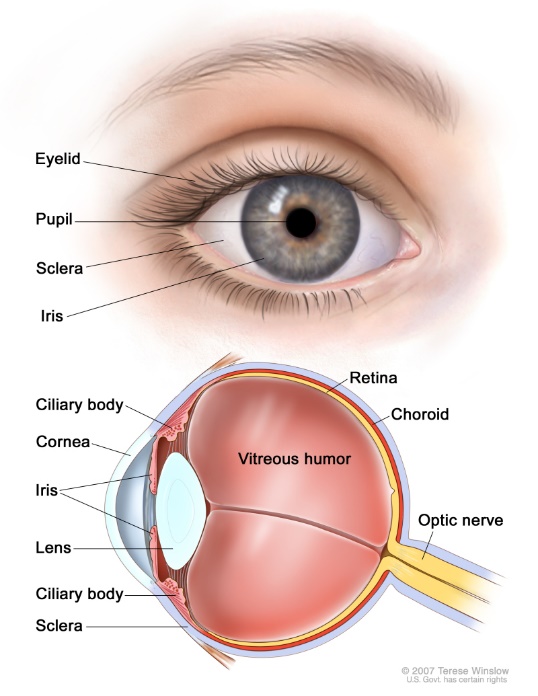
El melanoma ocular afecta con mayor frecuencia la capa media del ojo (la úvea), que incluye la parte coloreada (el iris), las fibras musculares alrededor del cristalino (cuerpo ciliar) y la capa de vasos sanguíneos que recubre la parte posterior del ojo (coroides).
El melanoma también puede desarrollarse en la conjuntiva, el tejido transparente que cubre la parte blanca del ojo y el interior de los párpados.
El melanoma que se desarrolla en la coroides, el iris o el cuerpo ciliar se denomina melanoma uveal, y el melanoma que se desarrolla en la conjuntiva se denomina melanoma conjuntival. Aunque ambos se desarrollan en el ojo, estas dos enfermedades son biológica y clínicamente diferentes entre sí, y ambas son muy diferentes de la forma más común de melanoma que se presenta en la piel. Debido a que la mayoría de los casos de melanoma ocular son uveales, a veces las personas se refieren al melanoma ocular como uveal.
Ambos tipos de melanoma ocular son poco frecuentes. El melanoma uveal se diagnostica en aproximadamente 2,500 personas cada año en los EE. UU., pero es el cáncer primario de ojo más común en adultos. La edad media de aparición es de aproximadamente 60 años, pero puede ocurrir a cualquier edad. El melanoma conjuntival es aún más raro y probablemente incidencia de < 1 casos por millón de personas.
Melanoma uveal
Algunos casos de melanoma uveal se diagnostican durante un examen ocular de rutina sin que el paciente presente síntomas, otros pacientes desarrollan síntomas que los llevan a hacerse un examen ocular y algunos pacientes presentan una peca en la coroides que se sigue y cambia con el tiempo. Los tratamientos más comunes para el melanoma uveal son las placas radioactivas, la terapia con haz de protones o la extirpación del ojo. El tratamiento primario del melanoma uveal es muy eficaz con reaparición en el ojo que ocurre en menos del 5% de los casos. Sin embargo, a pesar de la Si se controla el melanoma, existe el riesgo de que vuelva a aparecer fuera del ojo. El riesgo de que vuelva a aparecer se puede calcular a partir del tamaño del melanoma y de otros factores clínicos y patológicos; observando los cambios en los cromosomas del tumor (es decir, mediante pruebas citogenéticas); y observando un patrón alterado de los genes que se expresan (es decir, mediante el perfil de expresión génica).
Aproximadamente el 50 % de las personas con melanoma uveal desarrollarán metástasis. Cuando el melanoma uveal vuelve a aparecer, suele hacerlo en el hígado. El melanoma uveal avanzado es un cáncer difícil de tratar y se puede utilizar una amplia gama de tratamientos, entre ellos: inmunoterapia, agentes dirigidos molecularmente y una serie de tratamientos dirigidos al hígado, como embolización blanda, quimioembolización, inmunoembolización, radioembolización e infusión de quimioterapia en el hígado. pronóstico Para los pacientes con melanoma uveal metastásico, históricamente el tratamiento ha sido bastante pobre, con una supervivencia general limitada.
La buena noticia para los pacientes uveales es que en enero de 2022, la Administración de Alimentos y Medicamentos de EE. UU. (FDA) aprobó Kimtrak (tebentafusp-tebn) para el tratamiento de pacientes adultos con melanoma uveal irresecable o metastásico, que sean positivos para HLA-A*02:01. Kimmtrak es la primera y única terapia aprobada por la FDA para el tratamiento del melanoma uveal irresecable o metastásico (mUM). La aprobación de la FDA se basó en los resultados de un ensayo de fase 3. ensayo clínico en el que Kimmtrak mostró un beneficio de supervivencia general estadística y clínicamente significativo para los pacientes con mUM. Un total de 378 pacientes no tratados previamente fueron asignados aleatoriamente al grupo de Kimmtrak (tebentafusp) (252 pacientes) o al grupo de grupo de control (126 pacientes). El grupo de control recibió tratamiento con un solo agente: pembrolizumab (82% de los pacientes de control), ipilimumab (13%) o dacarbazina (6%). La supervivencia global (SG) al año fue del 73% en el grupo de tebentafusp y del 59% en el grupo de control.
Haga clic aquí para obtener más información sobre Kimmtrak.
Melanoma conjuntival
El melanoma conjuntival es más raro que el melanoma uveal. No tiene una causa clara y suele aparecer como una mancha pigmentada en la superficie externa del ojo. Las personas a las que se les diagnostica melanoma conjuntival suelen tener una resección del melanoma por un oftalmólogo oncólogo y pueden recibir tratamientos adicionales en el ojo, como crioterapia, quimioterapia tópica o radiación. A pesar del tratamiento agresivo, el melanoma conjuntival primario puede volver a aparecer. A diferencia del melanoma uveal, que se propaga con mayor frecuencia al hígado, el melanoma conjuntival a menudo hace metástasis en el ojo. la linfa ganglios linfáticos y pulmón, su comportamiento es mucho más similar al del melanoma cutáneo. No existe una recomendación estándar para el tratamiento de pacientes con melanoma conjuntival avanzado, principalmente debido a la rareza de la enfermedad. Generalmente, estos pacientes son tratados de manera similar a los pacientes con melanoma cutáneo avanzado, utilizando inmunoterapia y terapia dirigida, si corresponde.
Conclusiones
A pesar de los avances significativos que se han logrado en nuestra comprensión del melanoma conjuntival y uveal, estas enfermedades siguen siendo difíciles de tratar. Para desarrollar tratamientos más exitosos, debemos apoyar los esfuerzos combinados entre los pacientes que enfrentan estas enfermedades, los médicos que los atienden y los investigadores clínicos y de laboratorio que trabajan para desarrollar nuevos tratamientos para el melanoma conjuntival y uveal. Es a través de este tipo de cooperación que podemos aumentar la educación y la concienciación sobre estas enfermedades raras y, en última instancia, identificar tratamientos nuevos, más efectivos y potencialmente curativos.

